August 31, 2025
Supraorbital Nerve Cryoneurolysis Techniques for Migraine Relief
Understanding the Supraorbital Nerve and Its Role in Migraines
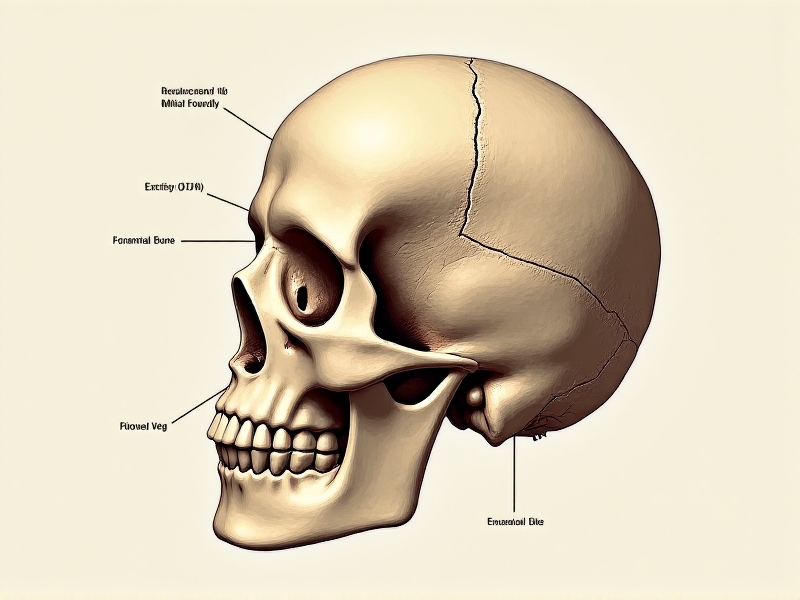
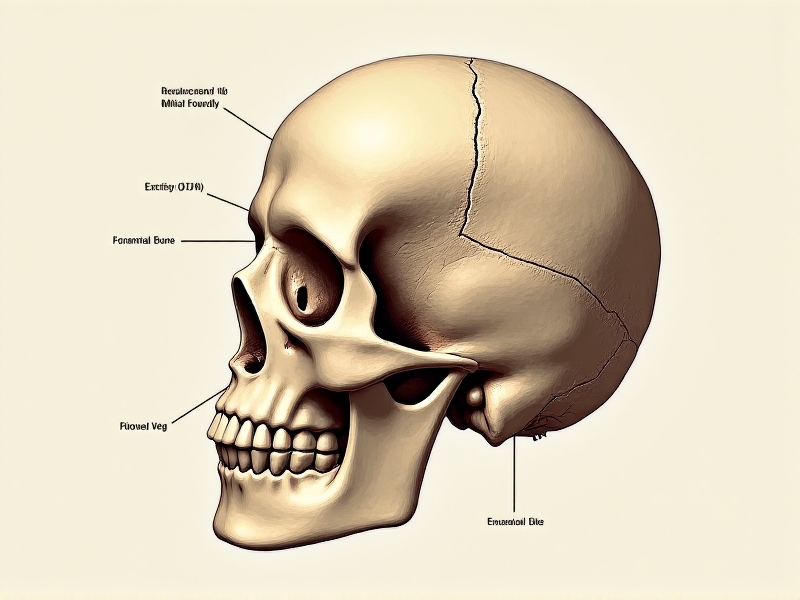
The supraorbital nerve, a branch of the ophthalmic division of the trigeminal nerve, plays a crucial role in the sensation of the forehead and scalp. This nerve is often implicated in migraine headaches, particularly those that manifest with pain in the frontal region. Migraines are a debilitating neurological condition characterized by severe, recurrent headaches often accompanied by nausea, vomiting, and sensitivity to light and sound. The exact pathophysiology of migraines is complex, but it is widely accepted that the activation and sensitization of the trigeminal nerve system, including the supraorbital nerve, contribute significantly to the pain experienced during a migraine attack.
Understanding the anatomy and function of the supraorbital nerve is essential for developing targeted treatments for migraines. The nerve exits the skull through the supraorbital foramen or notch, located just above the eye socket, and then branches out to innervate the forehead and scalp. When this nerve becomes irritated or inflamed, it can trigger or exacerbate migraine pain. Therefore, interventions that target the supraorbital nerve, such as cryoneurolysis, have garnered attention as potential methods for migraine relief.
What is Cryoneurolysis and How Does It Work?
Cryoneurolysis is a minimally invasive procedure that uses extreme cold to temporarily disrupt the function of targeted nerves, thereby reducing pain. The technique involves the application of a cryoprobe, which delivers controlled cooling to the nerve, causing it to freeze and become non-functional. This process, known as cryoablation, effectively blocks the transmission of pain signals from the affected nerve to the brain. The nerve is not permanently damaged; instead, it undergoes a process of Wallerian degeneration, after which it regenerates over time, typically within weeks to months.
The application of cryoneurolysis for migraine relief is based on the premise that by temporarily disabling the supraorbital nerve, the pain associated with migraines can be significantly reduced. The procedure is typically performed under local anesthesia and is considered safe, with minimal risk of complications. Patients often experience immediate relief following the procedure, and the effects can last for several months, providing a valuable window of reduced migraine frequency and severity.

The Evolution of Cryoneurolysis in Migraine Treatment
The use of cryoneurolysis for pain management is not new; it has been employed in various medical fields for decades. However, its application in the treatment of migraines is a relatively recent development. Early studies on cryoneurolysis focused on its use in managing chronic pain conditions such as post-surgical pain, arthritis, and neuropathic pain. The success of these studies paved the way for exploring its potential in migraine treatment, particularly for patients who have not responded well to conventional therapies.
Over the past decade, several clinical trials and case studies have demonstrated the efficacy of supraorbital nerve cryoneurolysis in reducing migraine frequency, severity, and duration. These studies have shown that the procedure is particularly beneficial for patients with chronic migraines, defined as experiencing headaches on 15 or more days per month. The evolution of cryoneurolysis techniques, including advancements in cryoprobe technology and imaging guidance, has further enhanced the precision and safety of the procedure, making it a viable option for a broader range of patients.

Patient Selection and Pre-Procedure Considerations
Not all migraine patients are suitable candidates for supraorbital nerve cryoneurolysis. Careful patient selection is crucial to ensure the best possible outcomes. Ideal candidates are those who have been diagnosed with chronic migraines and have not achieved adequate relief from standard treatments such as medications, lifestyle modifications, and other non-invasive therapies. A thorough medical history and physical examination are essential to rule out other potential causes of headaches and to confirm the involvement of the supraorbital nerve in the patient's migraine pattern.
Pre-procedure considerations include a detailed discussion of the potential risks and benefits of cryoneurolysis, as well as setting realistic expectations for the outcomes. Patients should be informed that while the procedure can provide significant relief, it is not a permanent cure for migraines, and the effects are temporary. Additionally, patients should be advised on the importance of continued migraine management strategies, such as avoiding triggers and maintaining a healthy lifestyle, to maximize the benefits of the procedure.
The Cryoneurolysis Procedure: Step-by-Step
The cryoneurolysis procedure for migraine relief is typically performed in an outpatient setting and takes about 30 to 60 minutes to complete. The patient is positioned comfortably, and the area around the supraorbital nerve is cleaned and sterilized. Local anesthesia is administered to numb the skin and underlying tissues, ensuring the patient's comfort throughout the procedure. Using imaging guidance, such as ultrasound, the physician identifies the precise location of the supraorbital nerve and positions the cryoprobe accordingly.
Once the cryoprobe is in place, it is activated to deliver controlled cooling to the nerve. The cooling process typically lasts for a few minutes, during which the nerve is exposed to temperatures cold enough to induce cryoablation. The patient may feel a sensation of cold or mild discomfort, but this is usually well-tolerated. After the procedure, the cryoprobe is removed, and the area is dressed with a small bandage. Patients are usually able to resume their normal activities immediately, although some may experience mild swelling or bruising at the treatment site.
Post-Procedure Care and Recovery
Following the cryoneurolysis procedure, patients are advised to take certain precautions to ensure a smooth recovery and to maximize the benefits of the treatment. Mild swelling, bruising, or tenderness at the treatment site is common and usually resolves within a few days. Patients may apply ice packs to the area to reduce swelling and discomfort. It is also important to avoid rubbing or applying pressure to the treated area to prevent irritation or infection.
Patients should be monitored for any signs of complications, such as excessive swelling, redness, or infection, although these are rare. Most patients experience immediate relief from migraine pain following the procedure, and the effects can last for several months. During this time, patients are encouraged to continue with their migraine management strategies, such as avoiding known triggers, maintaining a regular sleep schedule, and staying hydrated. Regular follow-up appointments with the physician are recommended to assess the long-term effectiveness of the treatment and to determine if additional sessions are needed.
Clinical Evidence Supporting Cryoneurolysis for Migraines
The efficacy of supraorbital nerve cryoneurolysis for migraine relief has been supported by a growing body of clinical evidence. Several studies have demonstrated significant reductions in migraine frequency, severity, and duration following the procedure. For example, a randomized controlled trial published in a leading neurology journal found that patients who underwent cryoneurolysis experienced a 50% reduction in migraine days per month compared to a control group. Additionally, patient-reported outcomes have shown improvements in quality of life, with many patients reporting decreased reliance on migraine medications and increased ability to participate in daily activities.
These findings are further supported by case studies and retrospective analyses, which have consistently reported positive outcomes for patients with chronic migraines. The procedure has also been shown to be well-tolerated, with a low incidence of adverse effects. While more research is needed to fully understand the long-term benefits and potential limitations of cryoneurolysis, the existing evidence suggests that it is a promising option for patients seeking alternative treatments for migraine relief.
Potential Risks and Complications
While cryoneurolysis is generally considered safe, as with any medical procedure, there are potential risks and complications that patients should be aware of. The most common side effects include temporary swelling, bruising, or tenderness at the treatment site, which typically resolve within a few days. In rare cases, patients may experience more serious complications, such as infection, nerve damage, or skin necrosis. However, these complications are uncommon and can often be mitigated by following proper procedural techniques and post-procedure care guidelines.
Patients should also be informed about the possibility of incomplete pain relief or the need for repeat procedures. While cryoneurolysis can provide significant relief for many patients, it is not a guaranteed cure for migraines, and individual responses to the treatment can vary. It is important for patients to have realistic expectations and to understand that cryoneurolysis is one component of a comprehensive migraine management plan. Open communication with the treating physician is essential to address any concerns and to ensure the best possible outcomes.
Comparing Cryoneurolysis to Other Migraine Treatments
Cryoneurolysis offers several advantages over other migraine treatments, particularly for patients who have not responded well to conventional therapies. Unlike medications, which can have systemic side effects and require daily use, cryoneurolysis is a localized treatment that targets the specific nerve involved in migraine pain. This targeted approach minimizes the risk of side effects and provides a more direct method of pain relief. Additionally, the effects of cryoneurolysis can last for several months, reducing the need for frequent interventions.
However, it is important to recognize that cryoneurolysis is not a one-size-fits-all solution and may not be suitable for all migraine patients. Other treatments, such as Botox injections, nerve blocks, and neuromodulation devices, may be more appropriate for certain individuals. The choice of treatment should be based on a thorough evaluation of the patient's medical history, migraine pattern, and treatment goals. In some cases, a combination of therapies may be the most effective approach to managing migraines.
Future Directions in Cryoneurolysis Research
As the field of cryoneurolysis continues to evolve, ongoing research is focused on optimizing the technique and expanding its applications in migraine treatment. One area of interest is the development of more advanced cryoprobes that allow for greater precision and control during the procedure. Additionally, researchers are exploring the use of cryoneurolysis in combination with other treatments, such as pharmacological therapies and neuromodulation, to enhance its effectiveness and provide longer-lasting relief.
Another promising direction is the investigation of biomarkers that can predict which patients are most likely to benefit from cryoneurolysis. By identifying specific characteristics or patterns in migraine patients, researchers hope to develop personalized treatment plans that maximize the chances of success. Furthermore, long-term studies are needed to better understand the durability of cryoneurolysis effects and to identify any potential risks associated with repeated procedures. As the evidence base continues to grow, cryoneurolysis is poised to become an increasingly important tool in the management of migraines.